Medical technology is rapidly evolving, making daily strides to improve patient care and health outcomes. At the heart of these improvements are sophisticated medical devices, from life-sustaining heart monitors to cutting-edge diagnostic tools. These devices extend lives and enhance the quality of life for countless patients across the globe, enabling more precise diagnoses, more effective treatments, and unparalleled monitoring capabilities.
Medical device engineers use their expertise to create and enhance medical technology. Their work provides patients with new freedoms and improved care. Device engineers work across various disciplines, like biomedical, electrical, and mechanical engineering, embodying the multidisciplinary nature of healthcare innovation.
However, these life-saving devices are far from perfect. Let’s examine some standard devices, their flaws, and how the future of medical technology might improve them.
Device #1: Medical Ventilators
Current Status
Ventilators push increased oxygen levels into the lungs and remove carbon dioxide from the body, mimicking natural breathing. They have long been life-saving technological systems, but the COVID-19 pandemic amplified their place in the public eye. During this time, ventilators helped countless patients in respiratory distress and those unable to breathe on their own due to illness, surgery, or trauma.
Despite their life-saving advantages, ventilators have shortcomings. They are typically bulky, requiring a dedicated space within intensive care units. Their cost can also be prohibitive, leaving hospitals with limited resources, particularly in rural or developing areas, inadequately equipped.
These machines are also complex, demanding highly trained, specialized personnel to operate and monitor them, adding another layer of challenge in settings where medical staff is in short supply. Additionally, the machines can be loud and uncomfortable, which can be distressing for patients and their families, potentially impeding their recovery.
Possible Innovations
As we imagine the next generation of ventilators, engineering has the power to transform patient care. Interest has surged around the creation of portable or even wearable ventilators. These mobile solutions could liberate patients from their beds, facilitating earlier mobility, which is crucial for recovery. They would also make ventilator therapy accessible in settings outside the traditional hospital ICU, from field hospitals to patient homes.
Cost drives accessibility. Simplified ventilator designs could significantly reduce costs, making it feasible for healthcare facilities with tighter budgets to afford these life-saving machines. Engineers could explore using less expensive materials or streamlined, easy-to-manufacture designs without compromising functionality and safety.
Automating ventilator operations could reduce the burden on healthcare staff and potentially improve patient outcomes. By incorporating sensors and advanced algorithms, ventilators could self-adjust to the patient's changing needs, ensuring optimal ventilation without constant manual recalibration. The vision includes innovative ventilators that integrate with hospital systems to provide real-time data analytics, aid clinical decision-making, and improve patient management.
Impact on Medical Ventilator Accessibility
These innovations have the potential to democratize access to crucial respiratory support. In low-resource settings or during healthcare crises when demand spikes unpredictably, having a stock of affordable, easy-to-use ventilators could be the difference between life and death for hundreds of individuals. More affordable ventilators enable rapid deployment and operation, possibly by less specialized staff, which is invaluable during a healthcare worker shortage.
By focusing on size, cost, and complexity reductions, engineers could play a pivotal role in ensuring that every patient who needs ventilatory support can receive it, regardless of location or local resources. This can bridge the gap in health equity and prepare global healthcare systems better for future pandemics or mass casualty events.
Device #2: Prosthetic Limb Technology
Current Status
Modern prosthetic limbs offer individuals with limb loss a chance to regain mobility and functionality. However, despite significant advancements in prosthetic technology, users still face considerable challenges. One of the main limitations is the lack of sensory feedback, which deprives users of the sense of touch and proprioception—the body’s ability to perceive its position in space. This can lead to difficulties in manipulating objects.
Many prosthetic limbs are heavier than the natural limbs they replace, contributing to user fatigue and discomfort. This can discourage wear and reduce the overall benefits that these devices intend to provide. Another major hurdle is cost; high-quality prosthetic limbs can be prohibitively expensive, limiting access for many who need them, especially in developing countries or individuals needing adequate insurance coverage.
Possible Innovations
Introducing haptic feedback mechanisms can revolutionize how users interact with their environment through prosthetic limbs. By incorporating systems that simulate touch, pressure, and even temperature, prosthetics could convey real-time sensory information to users, enhancing their ability to perform complex tasks and improving the psychological and neurological connection between the user and the prosthetic limb.
Developing lightweight materials such as advanced composites or utilizing innovative designs like those inspired by biological structures can result in prosthetics that are closer in weight to natural limbs. Reducing the weight will make prosthetics easier to use and wear, likely increasing user satisfaction and the frequency of use.
Cutting costs without sacrificing quality is paramount for widespread prosthetic access. Engineers can explore more affordable manufacturing processes, such as 3D printing, which lowers production costs and offers the added benefits of customization and rapid prototyping.
Implementing Artificial Intelligence (AI) can redefine the capabilities of prosthetic limbs. AI can facilitate more natural movement by learning and adapting to the user's behavior and movement patterns. Over time, the prosthetic could predict and perform the necessary movements to assist the user in everyday tasks, making the limb feel like a natural body extension. It could also adapt to changes in the user's lifestyle or body, ensuring the prosthetic remains a perfect fit over time.
Device #3 Insulin Pumps
Current Status
Insulin pumps are a cornerstone in the management of diabetes. They provide an alternative to multiple daily insulin injections for many individuals. Modern insulin pumps deliver insulin through a catheter placed under the skin, allowing for more precise blood sugar control.
Despite their effectiveness, current insulin pumps can be bulky and conspicuous, making them uncomfortable or inconvenient for patients to wear continuously. Manual adjustments to insulin dosing based on food intake and blood glucose levels can be time-consuming and error-prone. The infusion sites can also cause discomfort and, occasionally, skin infections or irritation.
Possible Innovations
Prospective advancements include AI-driven dosing, which leverages algorithms to analyze blood glucose data and continuously make instant dosing decisions. This smart dosing could reduce the burden of constant manual blood sugar management and help prevent hyperglycemia and hypoglycemia.
Integration with real-time health monitoring systems could further refine insulin delivery. By connecting with continuous glucose monitors (CGMs), insulin pumps could automatically adjust insulin doses based on glucose readings and predictive algorithms considering activity levels, sleep patterns, and meal data. This interconnected system would create a semi-closed loop system, reducing user input and making glucose control more seamless and less intrusive.
There's also a substantial opportunity to improve the physical design of insulin pumps, making them more discreet and comfortable for continuous wear. By utilizing advances in materials and electronics, future insulin pumps can slim down to the profile of a small patch, be worn invisibly under clothing, and cause minimal impact on a user's daily life.
Device #4: Wearable Health Monitors
Current Status
In recent years, wearable health monitors have become popular, largely thanks to their ability to track various health-related metrics continuously. Devices worn on the wrist or body measure basic parameters such as steps taken, heart rate, sleep quality, and sometimes blood oxygen saturation.
However, despite their popularity and utility, the current generation of wearable health monitors tends to be somewhat generic, offering a standardized set of measurements that might not meet everyone’s health or fitness monitoring needs. Their focus has primarily been on fitness tracking rather than comprehensive health monitoring, leaving significant room for improvement regarding the range and precision of health metrics they can track.
Possible Innovations
The future of wearable health monitors lies in their potential to track a much more extensive range of health metrics, offering a more personalized and comprehensive health monitoring experience. Innovations could include the ability to monitor blood glucose levels non-invasively, making life significantly more accessible for people with diabetes or those at risk of diabetes. Integrating sensors capable of tracking hydration levels could provide valuable data for athletes, those living in extreme climates, or individuals with specific health conditions that necessitate careful hydration management.
Detecting stress markers by measuring cortisol levels or other biochemical indicators could offer insights into a wearer’s mental well-being, opening the door for interventions to mitigate stress and its associated health risks. The ability to monitor a more comprehensive array of parameters like these could transform wearable health monitors into invaluable tools for predictive medicine, allowing for early detection and management of potential health issues.
Device #5: Kidney Dialysis Machines
Current Status
Traditional dialysis represents a lifeline for individuals with end-stage renal disease, performing the vital blood-filtering functions that their failing kidneys can no longer manage. However, patients typically need to spend upwards of four hours per session, three times a week, connected to large dialysis machines. These sessions are time-consuming and restrict patients' mobility, significantly impacting their quality of life. The stationary nature of these machines confines patients to dialysis centers or hospitals, placing considerable restrictions on their personal and professional lives and overall well-being.
Possible Innovations
Developing portable or implantable dialysis devices could represent a seismic shift in patient care, allowing users to do their daily activities with minimal interruption.
Portable Dialysis Machines: Portable dialysis technology aims to drastically reduce current systems' size and power requirements, enabling a device that can be comfortably worn or carried. This would allow patients to conduct their treatment on the go, even while they sleep, work, or engage in leisure activities. Such devices must balance efficiency, simplicity, and safety, ensuring users can manage their treatment without professional assistance.
Implantable Devices: Implantable dialysis machines are an even more ambitious goal. These devices would function within the body, continuously or on demand, to filter blood without needing external hookups. While significant technological and biological challenges remain in developing an implantable device, including power supply and biocompatibility, the potential to offer patients a near-normal lifestyle is a powerful motivator.
Wearable Artificial Kidneys (WAKs): Bridging the gap between portability and fully implantable, wearable artificial kidneys are a promising area of research. These devices aim to mimic the continuous filtration process of a functioning kidney, offering a more natural and less disruptive treatment regimen. Engineers play a crucial role in overcoming the challenges faced by WAKs, such as miniaturizing components without compromising their efficiency, developing non-thrombogenic materials to prevent blood clotting, and ensuring patients can wear the devices comfortably for extended periods.
The Role of Medical Device Engineers in Healthcare Innovation
Engineers are pivotal in healthcare innovation in the rapidly evolving medical technology landscape. Their expertise is instrumental in transforming conceptual ideas into tangible solutions that improve patient outcomes. Engineers from various disciplines—including biomedical, electrical, mechanical, and software engineering—bring diverse skills and perspectives that are critical in advancing the development of medical devices.
Contributions Across Disciplines
The complexity and diversity of medical devices, from wearable health monitors to dialysis machines, demand a broad range of engineering expertise. Biomedical engineers focus on the biological and medical aspects, ensuring that devices are compatible with human physiology and can effectively diagnose, monitor, or treat health conditions. Electrical and mechanical engineers design the hardware, sensors, and mechanics that make these devices operative and user-friendly. In contrast, software engineers develop the algorithms and data analysis tools that allow these devices to provide actionable insights to patients and healthcare providers.
Emphasizing Patient-Centered Design
A key element in the design and development of medical devices is the emphasis on patient-centered solutions. This approach prioritizes the patient's needs, experiences, and values, aiming to develop devices that are effective but also accessible, comfortable, and easy to use in daily life. Engineers must engage with patients, caregivers, and healthcare professionals throughout the development process to understand their needs and incorporate their feedback, ensuring that the final product enhances the quality of care and life for its users.
The Next Generation of Medical Device Engineers at Keck Graduate Institute
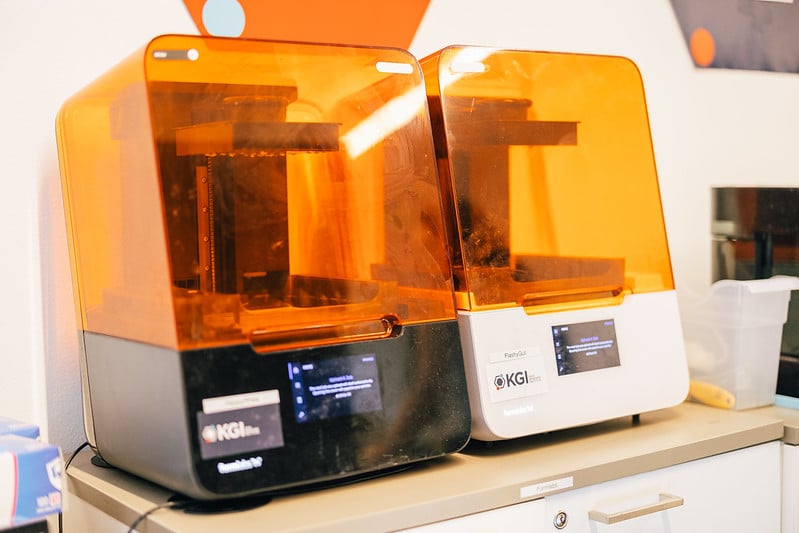
For aspiring engineers looking to make their mark in medical device development, the Master of Science in Medical Device Engineering program at Keck Graduate Institute (KGI) offers a unique opportunity. Keck Graduate Institute's program equips students with the interdisciplinary knowledge and hands-on experience necessary to lead medical device impact.
The program emphasizes project-based learning, allowing students to tackle real-world challenges in developing medical devices. This approach fosters technical expertise and critical skills in problem-solving, patient-centered design, and cross-disciplinary collaboration—preparing graduates to become leaders in creating groundbreaking healthcare solutions.
Request more information to learn more about a degree from Keck Graduate Institute. You can also connect with our admissions team.
Ready to start your career in medical devices? Apply to our Master of Science in Medical Device Engineering now.